MEDICINE BLENDED ASSIGNMENT (MAY)
MEDICINE BLENDED ASSIGNMENT (MAY)
I ( K Pranati, roll no 168) have been given the following cases to solve in an attmept to understand the topic of 'Patient clinical data analysis' to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and diagnosis and come up with a treatment plan.
This is the link of the questions asked regarding the cases:
http://medicinedepartment.blogspot.com/2021/05/online-blended-bimonthly-assignment.html?m=1
Below are my answers to the Medicine Assignment based on my comprehension of the cases.
NEUROLOGY
FIRST CASE
A 55year old male patient came to opd with c/o altered sensorium and involuntary movements from 11pm and recurrent episodes of seizures since 5yrs.
1. Is there any relationship between occurrence of seizure to brain stroke. If yes what is the mechanism behind it?
YES, there is a relationship between occurrence of seizure to brain stroke.
EARLY ONSET SEIZURES CAUSES:
During acute ischemic injury, accumulation of intracellular calcium and sodium may result in depolarization of the transmembrane potential, and other calcium-mediated effects. These local ionic shifts may lower the seizure threshold.
Glutamate excitotoxicity, is a well-established mechanism of cell death in the experimental stroke model.
The size of regional metabolic dysfunction may be relevant in causing early-onset seizures.
LATE ONSET SEIZURES CAUSES:
In late-onset seizures, persistent changes in neuronal excitability occur. Replacement of healthy cell parenchyma by neuroglia and immune cells may play a role in maintaining these changes.
Cortical location, is among the most reliable risk factors for poststroke seizures.
2. In the previous episodes of seizures, patient didn't loose his consciousness but in the recent episode he lost his consciousness what might be the reason?
A grand mal seizure causes a loss of consciousness and violent muscle contractions which the patient must have experienced in his last episode.
SECOND CASE
A 48-year-old gentleman hailing from a small town in Telangana presented to the casualty ward on 25th April 2021 at 7:40am with the chief complaints of unresponsiveness for 7 hours and 3 intermittent episodes of seizures in the past 3 hours.
1) What could have been the reason for this patient to develop ataxia in the past 1 year?
Ataxia usually results from damage to the part of your brain that controls muscle coordination (cerebellum). Considering the given history of the patient, the unattended head injuries and chronic alcoholism must have caused ataxia.
2) What was the reason for his IC bleed? Does Alcoholism contribute to bleeding diatheses ?
- The trauma resulting from falling
- injuries to head
- regular alcohol consumption
- high BP
Alcoholism causes a rise in blood pressure which may lead to bursting of vessels supplying the brain in turn leading to bleeding.
THIRD CASE
A 30 YEAR OLD MALE PATIENT LORRY DRIVER BY OCCUPATION CAME TO THE OPD WITH CHIEF COMPLAINTS OF
1. WEAKNESS OF RIGHT UPPERLIMB AND LOWER LIMB SINCE ONE DAY.
2.DEVIATION OF MOUTH TOWARDS LEFT SINCE ONE DAY.
1.Does the patient's history of road traffic accident have any role in his present condition?
I don't think the road traffic accident is of any significance as it took place several years ago.
2.What are warning signs of CVA?
3.What is the drug rationale in CVA?
- Mannitol is an osmotic agent and a free radical scavenger, which might decrease oedema and tissue damage in stroke.
- Ecosprin 75 tablet is an antiplatelet medicine and is also used to reduce the chances of formation of clot after.
- Atorva 40 Tablet belongs to a group of medicines called statins. It is used to lower cholesterol, and to reduce the risk of heart diseases. In my opinion, its purposeless to use it in this particular case since the cholesterol ,HDL,LDL levels are normal in the patient.
- Its proved in many studies, milk is associated with reduced risk of CVA.
4. Does alcohol has any role in his attack?
Liver damage due to too much alcohol, can stop the liver from making substances that help your blood to clot. This can increase your risk of having a stroke caused by bleeding in your brain.
5.Does his lipid profile has any role for his attack??
The lipid profile doesn't have any role in his attack since all the levels are in normal range.
FOURTH CASE
50-year-old male patient presented to hospital with complaints of weakness of all four limbs since 8 PM yesterday.
1)What is myelopathy hand ?
There is loss of power of adduction and extension of the ulnar two or three fingers ,and an inability to grip and release rapidly with these fingers. These changes have been termed "myelopathy hand" and appear to be due to pyramidal tract involvement.
2)What is finger escape ?
The finger escape sign - deficient adduction and/or, extension of the ulnar two or three fingers.
Finding of weak finger adduction in cervical myelopathy is also called as the "finger escape sign".
3)What is Hoffman’s reflex?
Hoffmann's reflex is a neurological examination finding elicited by a reflex test, which can help verify the presence or absence of issues arising from the corticospinal tract.
Hoffmann's reflex test involves loosely holding the middle finger and flicking the fingernail downward, allowing the middle finger to flick upward reflexively. A positive response is seen when there is flexion and adduction of the thumb on the same hand.
FIFTH CASE
A 40 year old male presented to the hospital from Yadagirigutta with the chief complaints of irrelevant talking and decreased food intake since 9 days.
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
EVOLUTION OF SYMPTOMATOLOGY:
12 YEARS AGO
- Addicted to alcohol, drinks about 3-4 quarters per day
2 YEARS AGO
- Diagnosed with type 2 Diabetes (irregular medication; once in 2 or 3 days)
1 YEAR AGO
- 1-2 episodes of seizures (mostly due to alcohol consumption)
4 MONTHS AGO
- Developed a seizure (mostly GTCS)
- Cessation of alcohol for 24 hours assosiated with symptoms of restlessness, sweating, and tremors.
10 DAYS AGO
- General body pains
9 DAYS AGO
- Started talking and laughing to himself (sudden onset)
- Decreased food intake
- Required assistance to move around
- Short term memory loss (couldn't recognise family members)
PRIMARY ETIOLOGY
- Wernicke's encephalopathy: thiamine deficiency secondary to alcohol dependence
- Uremic encephalopathy
- Altered sensorium: alcohol withdrawal syndrome
2) What are mechanism of action, indication and efficacy over placebo of each of the pharmacological and non pharmacological interventions used for this patient?
*DRUG NAME : syp potklor
MOA : It inceases the potassium levels
INDICATION : Hypokalemia
This medicine is used for the prevention or treatment of low potassium levels in the blood.
*DRUG NAME ; pregabalin
MOA : Although the mechanism of action has not been fully elucidated, studies involving structurally related drugs suggest that presynaptic binding of pregabalin to voltage-gated calcium channels is key to the antiseizure and antinociceptive effects observed in animal models.
INDICATION : Pregabalin is indicated for the management of neuropathic pain associated with diabetic peripheral neuropathy, postherpetic neuralgia, fibromyalgia, neuropathic pain associated with spinal cord injury, and as adjunctive therapy for the treatment of partial-onset seizures
EFFICACY OVER PREGABALIN :
P : 539
I : pregabalin
C : 265
O : the most common adverse events were dizziness and somnolence
GRBS: general randomized blood sugar
this test is also called capillary blood glucose assumes recent meals and therefore has higher reference values than fasting blood glucose.
*DRUG NAME : KCl
MOA : For use as an electrolyte replenisher and in the treatment of hypokalemia.
INDICATION : For use as an electrolyte replenisher and in the treatment of hypokalemia.
EFFICACY OVER KCl :
p : 18
i : KCl
c : random number of patients
o : amiloride might be more effective than potassium chloride in preventing hypokalaemia
INJ NS and RL : Lactated Ringer's is a sterile, nonpyrogenic solution for fluid and electrolyte replenishment and caloric supply in a single dose container for intravenous administration.
*DRUG NAME : lorazepam
MOA : Lorazepam allosterically binds on the benzodiazepine receptors in the post-synaptic GABA-A ligand-gated chloride channel in different sites of the central nervous system (CNS). This binding will result in an increase on the GABA inhibitory effects which is translated as an increase in the flow of chloride ions into the cell causing hyperpolarization and stabilization of the cellular plasma membrane.
INDICATION : Lorazepam is FDA-approved for the short-term relief of anxiety symptoms related to anxiety disorders and anxiety associated with depressive symptoms such as anxiety-associated insomnia. It is as well used as an anesthesia premedication in adults to relieve anxiety or to produce sedation/amnesia and for the treatment of status epilepticus.
EFFICACY OVER LORAZEPAM :
P : 56
I : lorazepam
C : 21
O : The effect size achieved in the placebo group was not inferior to that of benzodiazepines in general.
3) Why have neurological symptoms appeared this time, that were absent during withdrawal earlier? What could be a possible cause for this?
Patient had increased symptoms because he relapsed and drank alcohol again. Usually if you stop taking alcohol and start again patient will have severe withdrawal symtoms next time whenn he stops.
4) What is the reason for giving thiamine in this patient?
Wernicke’s encephalopathy is an acute neuropsychiatric disorder that occurs as a result of thiamine (vitamin B1) deficiency. Thiamine has been administered to counteract its deficiency.
5) What is the probable reason for kidney injury in this patient?
Chronic alcohol consumption might have lead to kidney injury in this patient.
6). What is the probable cause for the normocytic anemia?
The most common cause of normocytic anemia is a long-term (chronic) disease. In this case, the patient has been suffering from uremic encephalopathy which is an organic brain disorder. It develops in patients with acute or chronic renal failure, usually when the estimated glomerular filtration rate falls and remains below 15 mL/min.
7) Could chronic alcoholism have aggravated the foot ulcer formation? If yes, how and why?
Yes. Excessive alcohol can cause nutritional deficiencies and alcohol toxicity. These in turn can cause poor nutrition leading to poor wound healing and problems with the nerves (neuropathy). When the sensory nerves in the foot stop working, the foot can get injured and this leads to foot ulcers.
SIXTH CASE
A 52 year old male came to the hospital 2 days back presenting with slurring of speech and deviation of mouth that lasted for 1 day and resolved on the same day.
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
EVOLUTION OF SYMPTOMATOLOGY
7 DAYS AGO
Giddiness assosiated with an episode of vomiting
3 DAYS AGO
Giddiness - sudden in onset - continuous and gradually progressive -increased in severity upon getting up from the bed and while walking -associated with bilateral Hearing loss, aural fullness and presence of tinnitus
Vomiting (2-3 episodes per day), non projectile, non bilious containing food particles
Postural instability
ANATOMICAL LOCALIZATION
- Acute Cerebrovascular Accident- infarct in the right inferior cerebellar hemisphere.
- Cerebellar ataxia- inflammation in the occipital and temporal lobes of the cerebellum.
In this case, the patient has been diagnosed with cerebellar ataxia which in secondary to acute CVA.
2) What are mechanism of action, indication and efficacy over placebo of each of the pharmacological and non pharmacological interventions used for this patient?
- Ecosprin 75 mg Tablet is an anti-platelet medicine that contains acetylsalicylic acid (also known as Aspirin). It is used to prevent blood clot formation within the body. This tablet is also used to prevent heart attacks, stroke and heart-related chest pain (angina).
- Zofer is used for the associated vomiting.
- Statins are given to reduce the cholesterol.
- Clopidogrel prevents clot formation.
- Vertin Tablet is used to prevent and treat a disorder of the inner ear known as Ménière's disease. The symptoms include dizziness (vertigo), ringing in the ears (tinnitus), and loss of hearing, probably caused by fluid in the ear. This medicine helps relieve the symptoms by reducing the amount of fluid
3) Did the patients history of denovo HTN contribute to his current condition?
The patient's history of denovo HTN probably contributed to his current condition because long history andirregular medication can lead to peripheral neuropathy which in this case might've lead to cerebral atresia.
4) Does the patients history of alcoholism make him more susceptible to ischaemic or haemorrhagic type of stroke?
Alcohol may increase the risk of hemorrhagic stroke. Its caused by a blood clot blocking the flow of blood and oxygen from reaching the brain.
SEVENTH CASE
A 45 years old female ,house wife by occupation came to opd with chief complaints of palpitations, chest heaviness, pedal edema, chest pain, radiating pain along her left upper limb.
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
EVOLUTION OF SYMPTOMATOLOGY
10 YEARS AGO
Paralysis of both upper and lower limbs (right and left)
1 YEAR AGO
Right and left paresis due to hypokalemia
8 MONTHS AGO
Bilateral pedal edema - gradually progressing - present both in sitting and standing position - relieved on taking medication
Swelling over the legs (bilateral)
7 MONTHS AGO
Blood infection
2 MONTHS AGO
Treatment of neck pain
6 DAYS AGO
Pain - radiating along the the left upper limb - dragging in nature, aggrevated during palpitations - relieved by taking medication for palpitations
Chest pain associated with chest heaviness
5 DAYS AGO
Could feel her own heartbeat
Chestpain
Difficulty in breathing
Palpitations - since sudden in onset, more during night time - aggregated by lifting weights, speaking continuously - it is relieved by drinking more water and medication
Dyspnoea during palpitations (NHYA-CLASS-3)
ANATOMICAL LOCALISATION
Neurological system due to hypokalemia
PRIMARY ETIOLOGY
Electrolyte imbalance- hypokalemia
2) What are the reasons for recurrence of hypokalemia in her? Important risk factors for her hypokalemia?
Reason for recurrence of hypokalemia in this patient is due to recurrent hypokalemic periodic paralysis. The current risk factor is mainly due to administration of diuretics. Other risk factors are:
a) Abnormal loses due to medications, osmotic diuresis, renal tubular acidosis, hypomagnesemia.
b) Trance cellular shifts
c) Inadequate intake
d) Pseudohypokalemia
3) What are the changes seen in ECG in case of hypokalemia and associated symptoms?
ECG changes include:
- Flattening and inversion of T waves in mild hypokalemia
- Q-T interval prolongation
- Visible U wave and mild ST depression in more severe hypokalemia
- Severe hypokalemia can also result in arrhythmias such as Torsades de points and ventricular tachycardia.
Clinical symptoms of hypokalemia do not become evident until the serum potassium level is less than 3 mmol/L. The severity of symptoms also tends to be proportional to the degree and duration of hypokalemia.
The assosiated symptoms are:
- Muscle weakness (the pattern is ascending in nature affecting the lower extremities, progressing to involve the trunk and upper extremities and potentially advancing to paralysis).
- Fatigue
- Constipation
- Muscle twitches
- Palpitations
- Atrial or ventricular fibrillation
- Premature heartbeats
- Tachycardia
- Bradycardia
A 17 year old female student by occupation presented to causality on 1/5/2021 with chief complaints of involuntary movements of both upper and lower limbs a day before.
1) What can be the cause of her condition ?
Iron deficiency anemia might be the possible cause.
2) What are the risk factors for cortical vein thrombosis?
Risk factors for children and infants include:
- Beta-thalassemia major
- Heart disease — either congenital (you're born with it) or acquired (you develop it)
- Iron deficiency
- Certain infections
- Dehydration
- Head injury
- Sickle cell anemia
For newborns, a mother who had certain infections or a history of infertility
Risk factors for adults include:
- Pregnancy and the first few weeks after delivery
- Problems with blood clotting
- Collagen vascular diseases
- Obesity
- Cancer
- Inflammatory bowel disease like Crohn's
- Low blood pressure in the brain
3)There was seizure free period in between but again sudden episode of GTCS, why? Resolved spontaneously, why?
3 days after seizure free period patient was tapered off Midazolam, phenobarbitone. ThIs might be the cause of GTCS.
4) What drug was used in suspicion of cortical venous sinus thrombosis?
Clexane 0.4ml/sc was started in suspicion of CSVT
INFECTIOUS DISEASE AND HEPATOLOGY
FIRST CASE
A 55 year old male patient who is a palm tree climber by Occupation
came on 17th April 2021 with the chief Complaints of
PAIN ABDOMEN SINCE ONE WEEK
DECREASE APPETITE SINCE ONE WEEK
FEVER SINCE 2 DAYS
1. Do you think drinking locally made alcohol caused liver abscess in this patient due to predisposing factors present in it ? What could be the cause in this patient ?
Alcoholism, mainly consuming the locally prepared alcohol plays a major role as a predisposing factor for the formation of liver abscesses that is both amoebic as well as pyogenic liver abscess because of the adverse effects of alcohol over Liver. Hence, drinking locally made alcohol might be the cause of abscess in this patient.
2. What is the etiopathogenesis of liver abscess in a chronic alcoholic patient ? ( since 30 years - 1 bottle per day)
Alcohol can predispose to ALA through a multitude of mechanisms, including hepatic damage by alcohol, lowered body resistance and suppression of liver function due to poor nutritional status of habitual consumers of alcohol, increased presence of amoebae in the liquor prepared locally with poor regard to aseptic procedures, and depression of immune mechanisms in chronic alcoholics.
3. Is liver abscess more common in right lobe ?
Liver abscesses occur mostly in the right lobe of the liver (a more significant part with more blood supply), less commonly in the left liver lobe or caudate lobe.
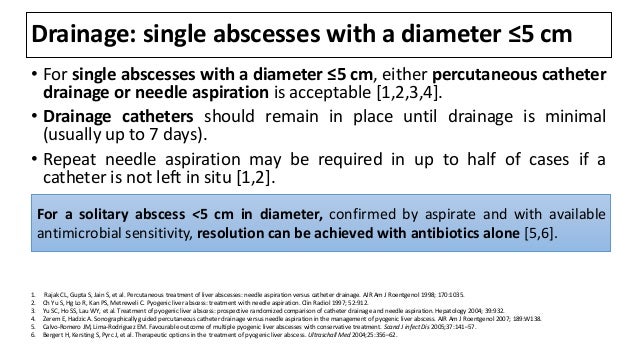
4.What are the indications for ultrasound guided aspiration of liver abscess ?
- complicated diverticular abscess.
- Crohn's disease related abscess.
- complicated appendicitis with appendicular abscess.
- tuboovarian abscess.
- post-surgical fluid collections.
- hepatic abscess (e.g. amoebic or post-operative)
- renal abscess or retroperitoneal abscess.
- splenic abscess.
SECOND CASE
A 21 yr old male student,resident of nakrekal, came to the hospital with the CHEIF COMPLAINTS: of abdominal pain since 20 days and fever since 18 days.
1) Cause of liver abcess in this patient ?
Since the patient has amoebic liver abscess it might be an infection that caused the abscess.
2) How do you approach this patient ?
Antibiotics are the considered approach since infection is thought to be the cause.
3)Why do we treat here ; both amoebic and pyogenic liver abscess?
If we dont treat amoebic liver abscess there is a chance that one of the following occurs:
Intraperitoneal, intrathoracic, or intrapericardial rupture, with or without secondary bacterial infection.
Direct extension to pleura or pericardium.
Dissemination and formation of brain abscess.
If we dont treat pyogenic liver abcsess there is a chance that one of the following occurs:
Sepsis.
Empyema resulting from contiguous spread or intrapleural rupture of abscess.
Rupture of abscess with resulting peritonitis.
Endophthalmitis when an abscess is associated with K pneumoniae bacteremia.
4) Is there a way to confirm the definitive diagnosis in this patient?
Same investigations as mentioned in the case.
PULMONOLOGY
FIRST CASE
A 55 year old female patient, a resident of Miryalaguda and farmer by occupation came to the hospital on 17/5/21 with the chief complaints of shortness of breath, pedal edema and facial puffiness.
https://
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
Evolution of symptomatology
20 years ago:
Shortness of breath : on of off while working at paddy field
relieved upon taking medication
12 years ago:
Episode of SOB : This one lasted 20 days and she had to be hospitalized. The SOB decreased upon treatment at the hospital.(grade II)
8 years ago
Similar episodes of SOB every year each lasting approximately 1 week. Relieved upon taking medication
Diabetes diagnosed
Polyuria
5 years ago:
Anemia treatment with iron injections
30 days back
Episode of SOB : insidious in onset and gradual in progression.
occurred on exertion and was relieved upon rest.
Generalised weakness
20 days back:
HRCT outside which showed bronchiectasis
Hyperstension diagnosed
15 days back:
Pedal edema : upto the level ankle
pitting type.
Facial puffiness
2 days back:
SOB :even at rest (grade IV)
not relieved with nebulizers
Drowsiness
ANATOMICAL LOCALIZATION
Chronic obstructive pulmonary syndrome
Bronchiectasis
COPD is caused by prolonged exposure to harmful particles or gases which may include second-hand smoke, environmental and occupational exposures, and alpha-1 antitrypsin deficiency. In this case patiemt is exposed to paddy frequently.
2) What are mechanism of action, indication and efficacy over placebo of each of the pharmacological and non pharmacological interventions used for this patient?
The elevation of the head of bed (HOB) to a semirecumbent position (at least 30 degrees) is associated with a decreased incidence of aspiration and ventilator-associated pneumonia (VAP)
During an exacerbation of COPD, give 24% or 28% oxygen via a Venturi facemask to patients with hypercapnia in order to maintain an oxygen saturation > 90%. In patients without hypercapnia, titrate the oxygen concentration upwards to keep the saturation > 90%.
BiPAP therapy targets these dysfunctional breathing patterns. By having a custom air pressure for when you inhale and a second custom air pressure when you exhale, the machine is able to provide relief to your overworked lungs and chest wall muscles.
DRUG NAME : augumentin
MOA : Amoxicillin competitively inhibits penicillin-binding protein 1 and other high molecular weight penicillin binding proteins. Penicillin bind proteins are responsible for glycosyltransferase and transpeptidase reactions that lead to cross-linking of D-alanine and D-aspartic acid in bacterial cell walls.Without the action of penicillin binding proteins, bacteria upregulate autolytic enzymes and are unable to build and repair the cell wall, leading to bacteriocidal action
INDICATION : Amoxicillin is given with calvulanic acid to treat acute bacterial sinusitis, community acquired pneumonia, lower respiratory tract infections, acute bacterial otitis media, skin and skin structure infections, and urinary tract infections.
EFFICACY OVER AUGUMENTIN :
P : 317
I : amoxicillin
C : 97
O : Treatment of ambulatory exacerbations of mild-to-moderate COPD with amoxicillin/clavulanate is more effective and significantly prolongs the time to the next exacerbation compared with placebo.
*DRUG NAME : Azithromycin
MOA : Azithromycin binds to the 23S rRNA of the bacterial 50S ribosomal subunit. It stops bacterial protein synthesis by inhibiting the transpeptidation/translocation step of protein synthesis and by inhibiting the assembly of the 50S ribosomal subunit . This results in the control of various bacterial infections . The strong affinity of macrolides, including azithromycin, for bacterial ribosomes, is consistent with their broad‐spectrum antibacterial activities
INDICATION : Azithromycin should be used only to treat or prevent infections that are proven or strongly suspected to be caused by susceptible bacteria in order to prevent the development antimicrobial resistance and maintain the efficacy of azithromycin
EFFICACY OVER AZITHROMYCIN:
P : 1142 patients
I : azithromycin
C : random number of patients
O : significant reduction in COPD exacerbations
Chest physiotherapy techniques such as intermittent positive pressure ventilation and positive expiratory pressure may benefit patients with COPD requiring assistance with sputum clearance, while walking programmes may have wider benefits for patients admitted with an exacerbation of COPD.
*DRUG NAME : hydrocortisone
MOA : The short term effects of corticosteroids are decreased vasodilation and permeability of capillaries, as well as decreased leukocyte migration to sites of inflammation.[A187463] Corticosteroids binding to the glucocorticoid receptor mediates changes in gene expression that lead to multiple downstream effects over hours to days
INDICATION : Hydrocortisone tablets are indicated for certain endocrine, rheumatic, collagen, allergic, ophthalmic, respiratory, hematologic, neoplastic, edematous, gastrointestinal, and other conditions
EFFICACY OVER HYDROCORTISONE :
P : 83
I : hydrocortisone
C : random number of patients
O : Corticosteroid treatment was associated with a significant reduction in the median duration of mechanical ventilation
3) What could be the causes for her current acute exacerbation?
Exacerbations of COPD are thought to be caused by complex interactions between the host, bacteria, viruses, and environmental pollution. These factors increase the inflammatory burden in the lower airways, overwhelming the protective anti‐inflammatory defences leading to tissue damage.
In this case, patient developed episodes commonly around January, while working in paddy field. dust particles in the paddy field or paddy can be the allergen that is causing the episodes.
4. Could the ATT have affected her symptoms? If so how?
Head elevation - increases hemodynamic performance and increases end expiratory lung volume
- Indications- .head injury, meningitis,pneumonia
Antibiotics
- INDICATIONS- severe exacerbations of COPD leading to hospitalization
- TAB. AUGUMENTIN - broad-spectrum antibacterial
- Formulation of Amoxicillin and Clavulanate Potassium
- TAB. AZITHROMYCIN - macrolide-type antibiotic
Diuretics
- INJ. LASIX IV – Furosemide
§ Loop Diuretic
§ Used to maintain blood pressure
Corticosteroids
-INJ. HYDROCORTISONE
(Relieve inflammation and decrease bronchospasm)
Nebulization
NEB. with IPRAVENT:
- Ipratropium Bromide – Bronchodilator
- Blocking cholinergic receptors
- decreases the production of cyclic guanosine monophosphate (cGMP)
- leading to relaxation of smooth muscles, and hence Bronchodilation
NEB. With BUDECORT:
- Budesonide- corticosteroid
-Used to control inflammation leading to bronchodilation
Other Bronchodilators
- TAB PULMOCLEAR - Acebrophylline and Acetylcysteine
-Airway mucus regulation and anti-inflammatory action causing bronchodilation
5.What could be the causes for her electrolyte imbalance?
Serum electrolyte imbalance such as hyponatremia, hypokalemia, hyperbilirubinemia, and elevated levels of transaminases, blood urea, and serum creatinine are either caused by the disease process or the therapy initiated
CARDIOLOGY
FIRST CASE
A 78 yr old male patient, resident of of kattangur and shepherd by occupation came to the OPD on 14 /5/2021 with chief complaints of:
- shortness of breath, since 20 days
- chest pain, since 20 days
- B/L pedal edema, since 4 days
- facial puffiness, since 4 days
1.What is the difference between heart failure with preserved ejection fraction and with reduced ejection fraction?
2.Why haven't we done pericardiocenetis in this pateint?
Pericardiocentesis is a procedure done to remove fluid that has built up in the sac around the pericardium. In this case, to keep a check if patient is having cardiac tamponade , review of ECHO has been done. As no cardiac tamponade was seen this procedure wasn't performed.
3.What are the risk factors for development of heart failure in the patient?
The risk factors of heart failure are:
Hypertension
Coronary artery disease
Diabetes
Certain medication
Alcohol abuse
Smoking
Obesity
Congenital heart defects
Sleep apnea
4.What could be the cause for hypotension in this case?
The patient is suffering from acute, rapid accumulation of fluid in the pericardium which causes signs of acute hemodynamic compromise in cardiac tamponade. Patients with this condition develop tachycardia, hypotension and distended neck veins.
SECOND CASE
A 73 yr male patient teacher by occupation, presented to OPD with chief complaints of :
Pedal edema, since 15 days
Shortness of breath, since 4 days
Decreased urine output, since 2 days
1.What are the possible causes for heart failure in this patient?
The probable causes for heart failure in this patient are:
- Chronic alcohol abuse
- Long standing case of hypertension (19 years)
- Stage 4 Chronic Kidney disease
2. What is the reason for anaemia in this case?
3.What is the reason for blebs and non healing ulcer in the legs of this patient?
Leg and foot ulcers in diabetic patients have three common underlying causes: venous insufficiency, peripheral neuropathy, or peripheral arterial occlusive disease.
4. What sequence of stages of diabetes has been noted in this patient?
STAGE1 DCBD insulin resistance
STAGE2 DCBD pre diabetes
STAGE3 DCBD type2
STAGE4 DCBD vascular complications includes retinopathy ,nephropathy, or neuropathy.
Here we see STAGE 4 due to diabetic neuropathy.
THIRD CASE
A 52yr old male came to the OPD with the chief complaints of decreased urine output and shortness of breath at rest since one day.
https://preityarlagadda.
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
EVOLUTION OF SYMPTOMATOLOGY
10 YEARS AGO
Surgery for inguinal hernia
3 YEARS AGO
Aggravated on and off pain at the site of surgery
On and off facial puffiness
1 YEAR AGO
Grade II shortness of breath - diagnosed for HTN (on medication)
2 DAYS AGO
Shortness of breath Grade II (on exertion)
Decreased urine output
Constipation
ONE DAY AGO
Shortness of breath Grade IV (at rest)
DAY OF ADMISSION
Anuria
ANATOMICAL LOCALISATION
1.HEART: a) Atrial fibrillation with Rapid ventricular response
b) Thrombi noted in Left Atrial Appendages and Left atrium
c) Dilated Main Pulmonary Artery and Left Pulmonary Arteries
d) Severe LV dysfunction
e) IVC dilated
2. KIDNEY: a) Cardiorenal syndrome
ETIOLOGY OF DISEASE IN PATIENT
Loss of Atrial contraction and Left atrial dilatation causes stasis of blood in the LA and may lead to thrombus formation in the Left Atrial Appendage. This predisposes patients to stroke and other forms of systemic embolism - Bilateral thrombosis
Cardiorenal syndrome 4 in this patient can be attributed to prior history of heart failure, HTN and age.
Abnormal heart rhythms, including atrial fibrillation or atrial flutter, affect 50 to 60 percent of all patients over 40 with an ASD.
2) What are mechanism of action, indication and efficacy over placebo of each of the pharmacological and non pharmacological interventions used for this patient?
1) Drug name: DOBUTAMINE
MOA: Dobutamine directly stimulates beta-1 receptors of the heart to increase myocardial contractility and stroke volume, resulting in increased cardiac output.
Indication: Indicated when parenteral therapy is necessary for inotropic support in the short-term treatment of patients with cardiac decompensation due to depressed contractility resulting either from organic heart disease or from cardiac surgical procedures.
Efficacy over dobutamine:
- P- 673 participants
- I - dobutamine
- c - out of 673 participants random number of patients are given placebo
- o - dobutamine is not associated with improved mortality in patients with heart failure, and there is a suggestion of increased mortality associated with its use
2) Drug name: CARVEDILOL
Mechanism of action: Carvedilol inhibits exercise induce tachycardia through its inhibition of beta adrenoceptors. Carvedilol's action on alpha-1 adrenergic receptors relaxes smooth muscle in vasculature, leading to reduced peripheral vascular resistance and an overall reduction in blood pressure.
Indication: Carvedilol is indicated to treat mild to severe heart failure, left ventricular dysfunction after myocardial infarction with ventricular ejection fraction or hypertension.
Efficacy over Carvedilol :
- p : 131
- i : carvedilol
- c : out of 131 participants random number of patients are given placebo
- o : The beta-blocker carvedilol can be safely employed in patients with severe heart failure. Improved left ventricular function
3) Drug name: UNFRACTIONED HEPARIN
MOA: Administered heparin binds reversibly to ATIII and leads to almost instantaneous inactivation of factors IIa and Xa The heparin-ATIII complex can also inactivate factors IX, XI, XII and plasmin. The mechanism of action of heparin is ATIII-dependent. It acts mainly by accelerating the rate of the neutralization of certain activated coagulation factors by antithrombin, but other mechanisms may also be involved. The antithrombotic effect of heparin is well correlated to the inhibition of factor Xa. Heparin is not a thrombolytic or fibrinolytic. It prevents progression of existing clots by inhibiting further clotting. The lysis of existing clots relies on endogenous thrombolytics.
Indication: It is used to prevent embolisms in patients with atrial fibrillation and as an adjunct antithrombin therapy in patients with unstable angina and/or non-Q wave myocardial infarctions
Efficacy over unfractioned heparin:
p : 1473
i : unfractioned heparin
c : out of 1473 participants random number of patients are given placebo
o : decrase in thromoembolism
4) Drug name: TAB. DYTOR
MOA: Torasemide is known to have an effect in the renin-angiotensin-aldosterone system by inhibiting the downstream cascade after the activation of angiotensin II. This inhibition will produce a secondary effect marked by the reduction of the expression of aldosterone synthase, TGF-B1 and thromboxane A2 and a reduction on the aldosterone receptor binding.
Indication: Torasemide is indicated for the treatment of edema associated with congestive heart failure, renal or hepatic diseases.
Efficacy over dytor:
p : 68
i : torsemide
c : 34
o : improvement in peripheral edema
5) Drug name: TAB. TAXIM
MOA: The bactericidal activity of cefotaxime results from the inhibition of cell wall synthesis via affinity for penicillin-binding proteins (PBPs). Cefotaxime shows high affinity for penicillin-binding proteins in the cell wall including PBP Ib and PBP III.
Indication: Used to treat gonorrhoea, meningitis, and severe infections including infections of the kidney (pyelonephritis) and urinary system. Also used before an operation to prevent infection after surgery
Efficacy over Taxim:
p : 60
i : taxim
c : out of 60 participants random number of patients are given placebo
o : the results indicate that cefixime twice daily is comparable in safety
6) Drug name: INJ THIAMINE
MOA: It is thought that the mechanism of action of thiamine on endothelial cells is related to a reduction in intracellular protein glycation by redirecting the glycolytic flux. Thiamine is mainly the transport form of the vitamin, while the active forms are phosphorylated thiamine derivatives. Natural derivatives of thiamine phosphate, such as thiamine monophosphate (ThMP), thiamine diphosphate (ThDP), also sometimes called thiamine pyrophosphate (TPP), thiamine triphosphate (ThTP), and thiamine triphosphate (AThTP), that act as coenzymes in addition to their each unique biological functions.
Indication: For the treatment of thiamine and niacin deficiency states, Korsakov's alcoholic psychosis, Wernicke-Korsakov syndrome, delirium, and peripheral neuritis.
Efficacy over thiamine:
P : 50
I : thiamine
C : 25
O : Thiamine was not associated to a significant reduction in vasopressor-free days over 7-days in comparison to placebo in patients with septic shock
3) What is the pathogenesis of renal involvement due to heart failure (cardio renal syndrome)? Which type of cardio renal syndrome is this patient?
Pathogenesis:
The development of CRS mainly focuses on the inability of the failing heart to generate forward flow, thus resulting in prerenal hypoperfusion. Inadequate renal afferent flow activates the RAAS, the sympathetic nervous system, and arginine vasopressin secretion, leading to fluid retention, increased preload, and worsening pump failure.
The patient is suffering from Type 4 CRS in which CKD leads to heart failure.
4) What are the risk factors for atherosclerosis in this patient?
- Hypertension
- Bad cholesterol levels
- Obesity
- Diabetes
- Lack of physical activity
- Age
- Smoking
5) Why was the patient asked to get those APTT, INR tests for review?
The patient was asked to get APTT and INR tests for review as he was prescribed TAB. Acitrom which is a blood thinner and can cause some common side effects such as unusual bleeding from the gums, heavy bleeding from cuts or wounds, unexplained bruising or nosebleeds, heavy periods, abdominal pain, blood vomiting, bloody or black tarry stools.
FOURTH CASE
A 67 year old female patient came to the OPD with C/O shortness of breath (SOB) since 1/2 hour.
https://
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
EVOLUTION OF SYMPTOMATOLOGY
12 YEARS AGO
Diagnosed with type 2 DM (on medication)
1 YEAR AGO
Heartburn like episodes (relieved without any medication)
7 MONTHS AGO
Diagnosed with TB (completed course of medication)
6 MONTHS AGO
Diagnosed with HTN (on medication)
NIGHT BEFORE ADMISSION
Sweating on exertion
Shortness of breath (at rest)
ON THE DAY OF ADMISSION
Shortness of breath since 1/2 an hour
ANATOMICAL LOCALISATION
PRIMARY ETIOLOGY
The increasing population in older age will lead to greater numbers of them presenting with acute coronary syndromes (ACS).he elderly are a high risk group with more significant treatment benefits than younger ACS. Nevertheless, age related inequalities in ACS care are recognised and persist.
2) What are mechanism of action, indication and efficacy over placebo of each of the pharmacological and non pharmacological interventions used for this patient?
1) Drug name: TAB METFORMIN
MOA: Metformin decreases blood glucose levels by decreasing hepatic glucose production, decreasing the intestinal absorption of glucose, and increasing insulin sensitivity by increasing peripheral glucose uptake and utilization.
Indication: Metformin is indicated as an adjunct to diet and exercise to increase glycemic control in adults and pediatric patients 10 years of age and older diagnosed with type 2 diabetes mellitus.
Efficacy over Metformin:
p : 451
i : metformin
c : out of 451 participants random number of patients are given placebo
o : Metformin improved glucose variables as compared with placebo.
3) What are the indications and contraindications for PCI?
Indications of PCI:
- Acute ST-elevation myocardial infarction
- Non–ST-elevation acute coronary syndrome
- Unstable angina
- Stable angina
- PCI is indicated for the critical coronary artery stenosis, which does not qualify for CABG
Contraindications of PCI:
- High bleeding risk
- Intolerance for oral antiplatelets long-term
- High-grade chronic kidney disease
- Critical left main stenosis with no collateral flow or patent bypass graft
- Chronic total occlusion of SVG
4) What happens if a PCI is performed in a patient who does not need it? What are the harms of overtreatment and why is research on overtesting and overtreatment important to current healthcare systems?
If PCI is performed in a patient who doesn't require it then one of the following may occur:
- Allergic reaction to the dye/contrast
- Kidney damage from the dye/contrast
- Injury/tears/ruptures of heart arteries
- Infection, bleeding or bruising at the catheter site
- Blood clots that can lead to stroke or heart attack
- Retroperitoneal bleeding
Harms of overtreatment:
- Psychological stress
- Financial toxicity
- Unnecessary care
- Surgical complications
- Loss of kidney function
- Unknown survival benefit
Overtesting, may cause harm to patients and the healthcare system, including through misdiagnosis, false positives, false negatives and overdiagnosis. Clinicians are ultimately responsible for test requests, and are therefore ideally positioned to prevent overtesting and its unintended consequences.
FIFTH CASE
A 60year old Male patient, resident of xxxxxxxx, came to the OPD with the Chief complaint of chest pain since 3 days and giddiness and profuse sweating since morning.
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
EVOLUTION OF SYMPTOMATOLOGY
5 DAYS AGO
first dose of COVISHEILD vaccine
3 DAYS AGO
Mild chest pain in the right side of the chest - pain was insidious in onset - gradually progressive - pain was of dragging type - radiating to the back
Dizziness was (not increasing or decreasing with change of position)
Profuse sweating
Disturbed sleep due to discomfort
ANATOMICAL LOCALIZATION
ETIOLOGY OF PATIENTS DISEASE
Hypertension and old age might be the probable etiology.
2) What are mechanism of action, indication and efficacy over placebo of each of the pharmacological and non pharmacological interventions used for this patient?
1) Drug name: ASPIRIN
MOA: Blocks prostaglandin synthesis. It is non-selective for COX-1 and COX-2 enzymes . Inhibition of COX-1 results in the inhibition of platelet aggregation
Indication: Due to its ability to inhibit platelet aggregation.
Reducing the risk of cardiovascular death in suspected cases of myocardial infarction (MI)
Efficacy over Aspirin:
p: 157 248
i : aspirin
c : out of 157248 participants random number of patients are given placebo
o : Aspirin was associated with a lower incidence of myocardial infarction. associated with an increased incidence of major bleeding
2) Drug name: TAB ATROVAS
MOA: Atorvastatin is a statin medication and a competitive inhibitor of the enzyme HMG-CoA (3-hydroxy-3-methylglutaryl coenzyme A) reductase, which catalyzes the conversion of HMG-CoA to mevalonate, an early rate-limiting step in cholesterol biosynthesis.
INDICATION : Atorvastatin is indicated, in combination with dietary modifications, to prevent cardiovascular events in patients with cardiac risk factors and/or abnormal lipid profiles. Atorvastatin can be used as a preventive agent for myocardial infarction, stroke, revascularization, and angina, in patients without coronary heart disease but with multiple risk factors and in patients with type 2 diabetes without coronary heart disease but multiple risk factors.
Efficacy over Atrovas:
p : 60
i: atrovastin
c : 42
o : Atorvastatin lowered LDL-C, apoB, and atherogenic lipoprotein subparticles in children with T1D and elevated LDL-C without worsening insulin resistance. The drug was well tolerated and safe. Long-term studies would provide better insight on the impact of these interventions in the development of cardiovascular disease in children with diabetes.
3) Drug name: TAB CLOPIB (active metabolite of clopidogrel)
MOA: Clopidogrel is metabolized to its active form by carboxylesterase-1. The active form is a platelet inhibitor that irreversibly binds to P2Y12 ADP receptors on platelets. This binding prevents ADP binding to P2Y12 receptors, activation of the glycoprotein GPIIb/IIIa complex, and platelet aggregation.
Indication: Clopidogrel is indicated to reduce the risk of myocardial infarction for patients with non-ST elevated acute coronary syndrome (ACS), patients with ST-elevated myocardial infarction, and in recent MI, stroke, or established peripheral arterial disease.
Efficacy over Clopib:
p : 79,613
i : clopidogrel
c : out of 79613 subject placebo is given to random subjects
o :clopidogrel was associated with a highly significant 14% proportional reduction in the risk of cardiovascular events
3) Did the secondary PTCA do any good to the patient or was it unnecessary?
Percutaneous transluminal coronary angioplasty is a surgical treatment to reopen a blocked coronary artery to restore blood flow. It is a type of percutaneous coronary intervention. When performed on patients with acute myocardial infarction, it is called primary angioplasty.
After the secondary PTCA the patient was doing better so it was necessary to do.
SIXTH CASE
An 87 year old male patient has presented with the complaints of shortness of breath since 3 days constipation since 3 days decreased urine output since 2 days.
1. How did the patient get relieved from his shortness of breath after i.v fluids administration by rural medical practitioner?
In this case one of the possibility is that patient might have received placebo.
2. What is the rationale of using torsemide in this patient?
Torsemide is used to reduce extra fluid in the body (edema) caused by conditions such as heart failure, liver disease, and kidney disease. This can lessen symptoms such as shortness of breath and swelling in your arms, legs, and abdomen. This drug is also used to treat high blood pressure.
3. Was the rationale for administration of ceftriaxone? Was it prophylactic or for the treatment of UTI?
Ceftriaxone is a 3rd generation cephalosporins which is commonly used for bacterial infections. So in this case ceftriaxone is used for tratement of UTI.
GASTROENTEROLOGY
FIRST CASE
A 33 yr old male daily wage labourer from miryalaguda who is a chronic alcoholic and smoker came to hospital on 30/04/2021 with CHEIF COMPLAINTS of pain abdomen & vomiting since 1 week and constipation, burning micturition, fever since 4 days.
https://63konakanchihyndavi.
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
EVOLUTION OF SYMPTOMATOLOGY
5 YEARS AGO
Pain in abdomen
Vomiting
(subsided by conservatibe treatment and abstinence of alcohol)
ONE YEAR AGO
Pain in abdomen and vomiting: 5-6 episodes
(resumed frequent intake of alcohol; conservative treatment by local RMP)
ONE WEEK AGO
Abdominal pain- 1) in umbilical, left hypochondriac, left lumbar and hypogastric region 2) throbbing type and radiating to back 3) assosiated with nausea and vomiting
Vomiting (one episode) - non bilious, non projectile, contains food particles and water
4 DAYS AGO
Fever
Constipation
Burning micturition
DURING HOSPITAL STAY
Developed progressive pneumothorax
ANATOMICAL LOCALISATION
PANCREAS- a) Acute on chronic pancreatitis b) Acute infective peri pancreatic fluid collections
LESSER SAC- a) Pseudocyst
LEFT LUNG- a) Moderate left pleural effusion with basal atelectasis
ETIOLOGY OF DISEASE IN PATIENT
The main cause of pancreatitis in this patient is attributed to the chronic intake of alcohol.
Recurrent episodes of pancreatitis has to lead to various complications of pseudocyst formation in lesser sac due to pancreatic duct rupture and BRONCHO PLEURAL FISTULA leading to pneumothorax.
2) What is the efficacy of drugs used along with other non pharmacological treatment modalities and how would you approach this patient as a treating physician?
Octreotide
The results of clinical investigations using somatostatin or its analogue are controversial, since all these trials had low statistical power. In a recent multicenter randomized controlled study with a large number of patients (n = 302) (and an adequate level of disease severity), no benefit of octreotide on progression or outcome was found. Chronic pancreatitis is characterized by an irreversible destruction of the exocrine and endocrine pancreatic parenchyma leading to maldigestion and diabetes. Pain, which may be caused by increased ductal pressure, is one of the most dominant symptoms in chronic pancreatitis. However, no beneficial effects on pain with pancreatic exocrine secretion-inhibiting drugs have been demonstrated. Treatment of other complications of the disease (pseudocyst formation, fistula and pancreatic ascites), with somatostatin or octreotide has given conflicting results. However, in a prophylactic clinical setting (e.g. elective pancreatic surgery) the inhibition of exocrine pancreatic secretion reduces complications.
A clinical and therapeutical study of 47 patients with the diagnosis of acute pancreatitis is reported. According to Ranson's criteria patients were initially classified as suffering from mild (28) and severe (18) acute pancreatitis. Twenty-eight, 11, 7 and 1 patients had biliary, alcoholic, idiopathic and neoplastic causes, respectively, of their conditions. The classification of episodes was made on the basis of clinical manifestations, biologic investigations, and imaging diagnosis, and is shown in the corresponding tables. The therapeutic profile was a randomized double-blind study: perfused somatostatin (SS) versus placebo (P) (physiologic saline 0.9%). The administration of somatostatin in perfusion (250 mcg/h/48 hours) did not improve significantly the parameters used to score the severity, although the mortality rate decreased significantly (p < 0.05) in the group of patients with the severe form of the disease.
Antibiotics
The mortality rates were 5.26% (5/95) and 18.18% (16/88) in prophylactic antibiotics and placebo/none-treatment groups, respectively.
Material and methods: Seventy-three patients with severe pancreatitis were included in a prospective, randomized, clinical study in seven Norwegian hospitals. The number of patients was limited to 73 because of slow patient accrual. Severe pancreatitis was defined as a C-reactive protein (CRP) level of >120 mg/l after 24 h or CRP >200 48 h after the start of symptoms. The patients were randomized to either early antibiotic treatment (imipenem 0.5 g x 3 for 5-7 days) (imipenem group) (n=36) or no antibiotics (control group) (n=37).
Results: The groups were similar in age, cause of pancreatitis, duration of symptoms and APACHE II score. Patients in the imipenem group experienced lower rates of complications (12 versus 22 patients) (p=0.035) and infections (5 versus 16 patients) (p=0.009) than those in the control group. There was no difference in length of hospital stay (18 versus 22 days), need of intensive care (8 versus 7 patients), need of acute interventions (10 versus 13), nor for surgery (3 versus 3) or 30-day mortality rates (3 versus 4).
Conclusions: The study, although underpowered, supports the use of early prophylactic treatment with imipenem in order to
https://pubmed.ncbi.nlm.nih.gov/17506001/
TPN
The aim of the study was to evaluate and control the therapeutic validity of Somatostatin administration and the clinical benefits of parenteral nutrition during acute pancreatitis. We selected 31 patients with 1st and 2nd degree pancreatitis according to Ranson's classification. Diagnosis was based on clinical and humoral data and confirmed by echography and CT examinations. The most common etiological cause was biliary++ lithiasis (74.2%). All the patients in the study were split into two groups and received conventional treatment. The therapeutic schedule administered to group 1 included somatostatin (250 micrograms/h for 72-96 h), while group 2 received total parenteral nutrition with 2,000-2,500 Kal/day trough a central vein. The data obtained from our study demonstrated that both somatostatin and parenteral nutrition are valid tools during the acute phase of the disease. It must be pointed out that the former significantly influences the clinical course and allows a precise control of the painful symptomatology, the objective picture and the curve of the main hematochemical parameters. Parenteral nutrition betters the anabolic response of the organism during the acute phase and carries out an indirect antienzymatic response, so favouring a quicker recovery than observed in the group treated with somatostatin.
https://pubmed.ncbi.nlm.nih.gov/2566958/
USG drain
A single-center retrospective study was performed after obtaining Institutional review board approval for analyzing hospital records of patients with acute necrotizing pancreatitis from January 2012 to July 2017. Seventy-eight consecutive patients with necrotizing pancreatitis and acute necrotic collections (ANC) were managed with percutaneous catheter drainage (PCD) and catheter-directed necrosectomy, in early phase of the disease (< 21 days). Clinical data and laboratory parameters of the included patients were evaluated until discharge from hospital, or mortality.
Results
Overall survival rate was 73.1%. Forty-two (53.8%) patients survived with PCD alone, while the remaining 15 (19.2%) survivors needed additional necrosectomy. The timing of intervention from the start of the hospitalization to drainage was 14.3 ± 2.4 days. Significant risk factors for mortality were the presence of organ system failure, need for mechanical ventilation, renal replacement therapy, and the acute physiology and chronic health evaluation II (APACHE II) score. An APACHE II score cutoff value of 15 was a significant discriminant for predicting survival with catheter-directed necrosectomy.
Conclusion
An early PCD of ANC in clinically deteriorating patients with acute necrotizing pancreatitis, along with aggressive catheter-directed necrosectomy can avoid surgical interventions, and improve outcome in a significant proportion of patients with acute necrotizing pancreatitis.
https://link.springer.com/article/10.1007/s12664-019-00969-0
SECOND CASE
Case of 52 year old man with severe epigastric pain.
1) What is causing the patient's dyspnea? How is it related to pancreatitis?
In the pathogenesis of respiratory complications of pancreatitis, inflammatory mediators released from pancreatic injury and digestive actions of pancreatic enzymes play a key role. The role of active digestive enzymes in circulation, release of multiple pro-inflammatory cytokines, activation and migration of leukocytes/neutrophils, complement mediated injury, and platelet activating factors are primarily involved in development of these complication. A damage to the pulmonary vasculature caused by activated trypsin leads to increased endothelial permeability while the main culprit for pulmonary complications.
2) Name possible reasons why the patient has developed a state of hyperglycemia.
Pancreatitis damages the alpha and beta cells that produce glucagon and insulin which are the hormones that control the amount of sugar in the blood. This can lead to an increase in blood sugar levels causing hyperglycemia.
3) What is the reason for his elevated LFTs? Is there a specific marker for Alcoholic Fatty Liver disease?
According to the report the patient has grade I fatty livver due to his chronic consumption of alcohol which might've caused elevated LFT's.
The biochemical markers for chronic alcohol consumption that have been most commonly studied are serum GGT, AST, ALT, mean corpuscular volume (MCV) and carbohydrate-deficient transferrin (CDT). An AST to ALT ratio over 2 is highly suggestive of ALD. Most patients with non-ALD have AST to ALT ratios below one. Specific IgA antibodies directed towards acetaldehyde-derived protein modifications are frequently seen alcoholics and thus IgA levels are increased in chronic ALD. An increased ratio of IgA to IgG is highly suggestive of ALD.
Chronic alcohol consumption is known to induce a rise in serum GGT and is a widely used index for excessive alcohol use. However, elevated GGT alone has both low sensitivity and specificity for alcohol abuse. GGT is not specific to alcoholism and is increased in many conditions such as obesity, advanced age, moderate alcohol consumption, all forms of liver disease including fatty liver and in particular intra and extrahepatic biliary obstruction, hepatocellular carcinoma and phenytoin use. The sensitivity of GGT as a marker for alcohol consumption in young adults has been showed to be particularly poor even in cases of documented alcohol dependence.
https://www.ncbi.nlm.nih.gov/
4) What is the line of treatment in this patient?
Treatment:
• IVF: 125 mL/hr
• Inj PAN 40mg i.v OD
• Inj ZOFER 4mg i.v sos
• Inj Tramadol 1 amp in 100 mL NS, i.v sos
• Tab Dolo 650mg sos
• GRBS charting 6th hourly
• BP charting 8th hourly
THIRD CASE
A 45 year old Female patient, came to Hospital with cheif complaints of:
Fever since 3 days
Pain in abdomen since 2 days
Decreased urine output since 2 days
Abdominal distention since morning
https://chennabhavana.
1) What is the most probable diagnosis in this patient?
The probable diagnosis in this case is Analgesic Nephropathy.
2) What was the cause of her death?
The cause of death in this may be due to sepsis.
3) Does her NSAID abuse have something to do with her condition? How?
As the patient has Grade III RPD changes in her right kidney she may have an underlying CKD which is secondary to her NSAID abuse.
NEPHROLOGY AND UROLOGY
FIRST CASE
A 52 yr old male patient who is a farmer by occupation,
Presented to hospital on 17 May 2021 with Chief Complaints of
SOB since 4 days
Burning micturition since 4 days
Fever since 2 days
https://kavyasamudrala.
1. What could be the reason for his SOB ?
Anemia is an important cause of SOB in diabetic CKD patients.
2. Why does he have intermittent episodes of drowsiness ?
Its mainly due to hyponatremia because patient showed improvement after administration of sodium.
3. Why did he complaint of fleshy mass like passage in his urine?
The reaon might be pyuria causing the foamy fleshy mass appearance (pus cells appear like fleshy mass).
4. What are the complications of TURP that he may have had?
He seems to face electrolyte imbalance post TURP.
SECOND CASE
Informant is the Mother who complains of frequent urination in her otherwise bubbling child since 4 months.
1.Why is the child excessively hyperactive without much of social etiquettes ?
The child seems to be psycho somatic, hence the behaviour.
2. Why doesn't the child have the excessive urge of urination at night time ?
The child has excessive urge to urinate during the daytime even though the bladder isn't full because of his psychological impulse to urinate. During the night time he wouldn't have the compulsion to do so since he's asleep.
3. How would you want to manage the patient to relieve him of his symptoms?
I wouldn't recommend any medicines as such because all the reports, clinical findings seem normal. He could be counselled mentally and go to therapy to overcome his psychological compulsion to urinate excessive amount of times even when he doesn't need to. A placebo might be of help.
INFECTIOUS DISEASE (HI VIRUS, MYCOBACTERIA, GASTROENTEROLOGY, PULMONOLOGY)
A 40 year old lady who works in cotton fields came to the hospital with the chief complaints of :
DIFFICULT IN SWALLOWING,FEVER AND COUGH, SINCE 2 MONTHS
https://vyshnavikonakalla.
1.Which clinical history and physical findings are characteristic of tracheo esophageal fistula?
Characteristic clinical history of tracheoesophageal fistula are :
cough
difficulty in swallowing
loss of weight
shortness of breath
Characteristic physical findings of tracheoesophageal fistula are:
Fistulous communication between left main bronchus and mid thoracic oesophagus.
2) What are the chances of this patient developing immune reconstitution inflammatory syndrome? Can we prevent it?
As patient is TB positive, during or after completion of anti-TB therapy, there is a chance of developing tuberculosis immune reconstitution inflammatory syndrome.
The most effective prevention of immune reconstitution inflammatory syndrome would involve initiation of ART before the development of advanced immunosuppression.
INFECTIOUS DISEASE (MUCORMYCOSIS, OPHTHALMOLOGY, OTORHINOLARYNGOLOGY, NEUROLOGY)
50/Male who is a resident of choutuppal
Daily wage labourer by occupation
Came with chief complaints of
Fever since 10 days
Facial puffiness and periorbital edema since 4 days
Weakness of right upper limb and lower limb since 4 days
Altered sensorium since 2 days
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
EVOLUTION OF SYMPTOMATOLOGY
Fever, generalised weakness
↓
Facial puffiness, Periorbital edema
↓
Altered sensorium
↓
- Increased progression of periorbital edema
- Discharge from eye- blood tinged
- Worsening of patients response, drowsy
- Blackish discolouration of medial canthus of eye
ANATOMICAL LOCATION
PRANASAL SINUSES.
Other anatomical parts affected due to spread of disease are ORBITS and CEREBRAL CORTEX.
PRIMARY ETIOLOGY
Its likely due to a fungal infection caused by mucorales.
Hence, mucormycosis is primary cause of disease in the patient.
2) What is the efficacy of drugs used along with other non pharmacological treatment modalities and how would you approach this patient as a treating physician?
Mucormycosis is a serious infection and needs to be treated with prescription antifungal medicine, usually amphotericin B ,posaconazole, isavuconazole. These are given through a vein or by mouth.
3) What are the postulated reasons for a sudden apparent rise in the incidence of mucormycosis in India at this point of time?
- Uncontrolled diabetes HbA1C > 6.5%
- Steroid overuse due to COVID 19.
- Immunological alterations due to COVID 19 ↓CD4+/CD8+
- Secondary infection due to widespread use of antibiotics and steroids.
INFECTIOUS DISEASE (COVID 19)














Comments
Post a Comment