This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. Here we discuss our individual patient's problems through series of inputs from global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs. This E log book also reflects my patient-centred online learning portfolio and your valuable inputs on the comment box is welcome."I've been given this case to solve in an attempt to understand the topic of "patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with a diagnosis and treatment plan
K Pranati , roll no 168
CHIEF COMPLAINTS:
79 year old female came to the hospital with the complaints of
-lower back ache since 5 months
-With c/o burning sensation of both upper and lower limbs since 5 months
-Pain during defecation since 5 months
-fever since 10 days
HOPI:
Patient was apparently asymptomatic 5 months back. Then she complained of lower back ache which was insidious in onset,gradually progressive aggravated on bending and is relieved on medication.
She developed burning sensation of both UL and LL since 5 months which is not associated with any tingling and numbness of the limbs.
She also complaints of burning micturition since 5-6 months, nocturia present and pain during defecation which is non blood stained.
Since 10 days she complaints of low grade fever which is not associated with chills and rigor,on and off with no cough and cold.
GENERAL EXAMINATION:
Patient is conscious coherent and cooperative
No pallor ,icterus , clubbing,cyanosis,lymphadenopathy ,pedal
VITALS
BP- 130/100mmhg
PR -88bpm
RR-19cpm
Spo2 99% at room air
Temperature -98.2f
SYSTEMIC EXAMINATION:
CVS: s1,s2 heard ,no Murmurs,jvp not raised
RS: BAE,no added sounds ,NVBS,
P/A: obese,soft, non tender,bowel sounds can be heard
CNS:
Pt is conscious
Speech is normal
No meningeal signs
Normal cranial nerve examination, motor system, sensory system
GCS: E4,V5,M6
Reflexes:
R L
B ++ ++
T ++ ++
S ++ ++
K ++ ++
A ++ ++
P Flexor Flexor
CLINICAL IMAGES
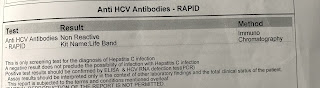
INVESTIGATIONS(26/5/2023)
PROVISIONLA DIAGNOSIS
-LUMBAR SPONDYLOSIS
-PERIPHERAL NEUROPATHY
-GRADE 2-3 HAEMERROIDS
-CKD
TREATMENT
1.IV FLUIDS NS/RL @ 50ml/hr
2.INJ.LASIX 40mg IV/BD
3.INJ.HAI according to GRBS
4.TAB.NODOSIS 500mg po/bd
5.TAB.DOLO 650mg Po/SOS
6.SYP.CREMAFFIN PLUS PO/HS
SUMMARY
75 year old female came with c/o lower back ache , burning sensation in both upper limbs and lower limbs and pain during defecation since 5months
GENERAL EXAMINATION:
Patient is conscious coherent and cooperative
No pallor ,icterus , clubbing,cyanosis,lymphadenopathy ,pedal
VITALS
BP- 130/100mmhg
PR -88bpm
RR-19cpm
Spo2 99% at room air
Temperature -98.2f
SYSTEMIC EXAMINATION:
CVS: s1,s2 heard ,no Murmurs,jvp not raised
RS: BAE,no added sounds ,NVBS,
P/A: obese,soft, non tender,bowel sounds can be heard
CNS:
Pt is conscious
Speech is normal
No meningeal signs
Normal cranial nerve examination, motor system, sensory system
GCS: E4,V5,M6
Reflexes:
R L
B ++ ++
T ++ ++
S ++ ++
K ++ ++
A ++ ++
P Flexor Flexor
PROVISIONLA DIAGNOSIS
-LUMBAR SPONDYLOSIS
-PERIPHERAL NEUROPATHY
-GRADE 2-3 HAEMERROIDS
-CKD
TREATMENT
1.IV FLUIDS NS/RL @ 50ml/hr
2.INJ.LASIX 40mg IV/BD
3.INJ.HAI according to GRBS
4.TAB.NODOSIS 500mg po/bd
5.TAB.DOLO 650mg Po/SOS
6.SYP.CREMAFFIN PLUS PO/HS











Comments
Post a Comment